This site is intended for Healthcare Professionals only. if you are a member of the general public, click here
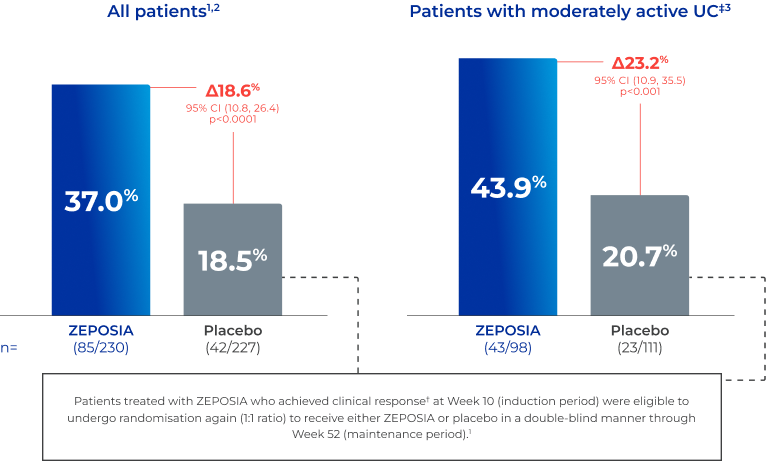
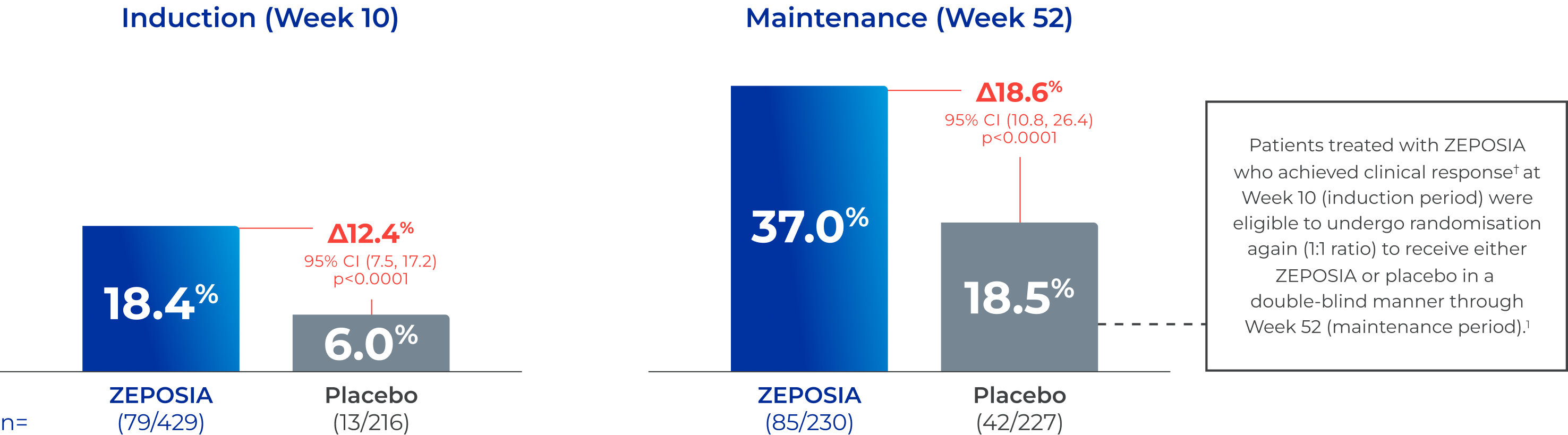
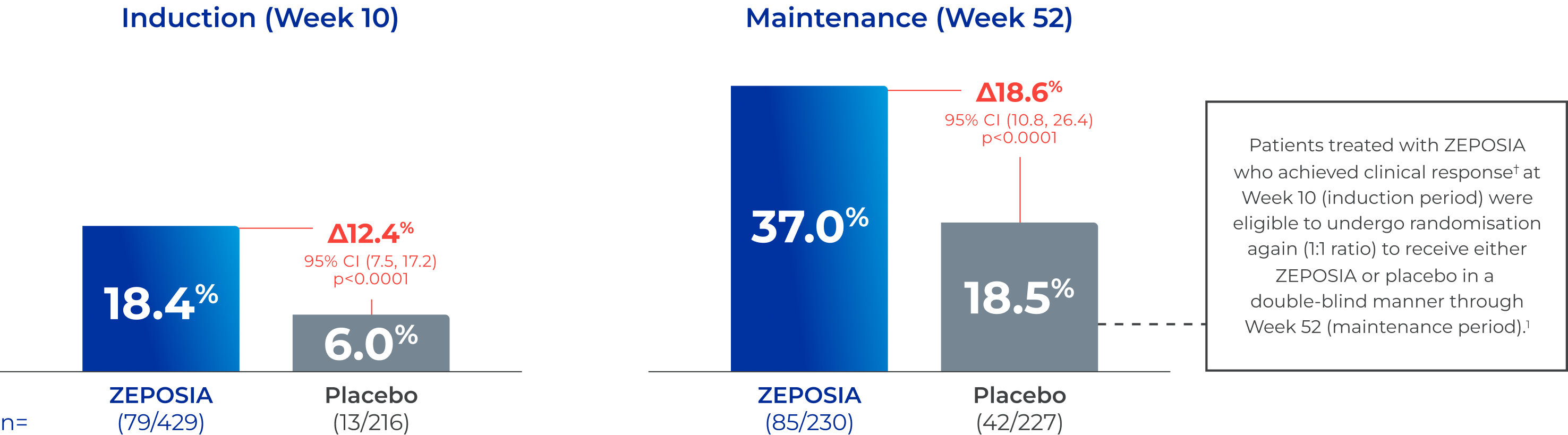
Significantly more patients achieved clinical remission* with ZEPOSIA
at Week 10 and at Week 52 vs placebo1,2
 Pinch & zoom to explore
Pinch & zoom to explore
Adapted from Sandborn WJ et al. 2021.1
*Clinical remission was assessed using the 3-component Mayo score and defined as a RBS of 0; a SFS of 1 or less, with a decrease of at least 1 point from baseline; and an endoscopy subscore of 1 or less without friability (all on scales from 0 [none] to 3 [most severe]).1,2
†Clinical response was defined as a reduction from baseline in the 9-point Mayo score of ≥2 points and ≥35%, and a reduction from baseline in the RBS of ≥1 point or an absolute RBS of ≤1 point.2
CI, confidence interval; RBS, rectal-bleeding subscore; SFS, stool-frequency subscore.
Adapted from Sandborn WJ et al. 20211 & Peyrin-Biroulet L et al. 2022.3
This was a post-hoc analysis and should be interpreted with caution. The results for individual subgroups are not powered to draw meaningful conclusions and should therefore be interpreted with caution.
*Clinical remission was assessed using the 3-component Mayo score and defined as a RBS of 0; a SFS of 1 or less, with a decrease of at least 1 point from baseline; and an endoscopy subscore of 1 or less without friability (all on scales from 0 [none] to 3 [most severe]).1,2
†Clinical response was defined as a reduction from baseline in the 9-point Mayo score of ≥2 points and ≥35%, and a reduction from baseline in the RBS of ≥1 point or an absolute RBS of ≤1 point.2
‡Of the total TRUE NORTH population (N=1,012) at baseline, 39.8% (n=403) of patients had moderate disease and 60.2% (n=609) had severe disease (defined as Mayo endoscopic score of 3).3
CI, confidence interval; RBS, rectal-bleeding subscore; SFS, stool-frequency subscore; UC, ulcerative colitis.
References
- Sandborn WJ et al. N Engl J Med. 2021;385(14):1280–1291.
- ZEPOSIA (ozanimod) Summary of Product Characteristics, 2023.
- Peyrin-Biroulet L et al. Poster presented at: United European Gastroenterology Week 2022; Vienna, Austria, and Virtual; 8–11 October, 2022. Poster: MP247.